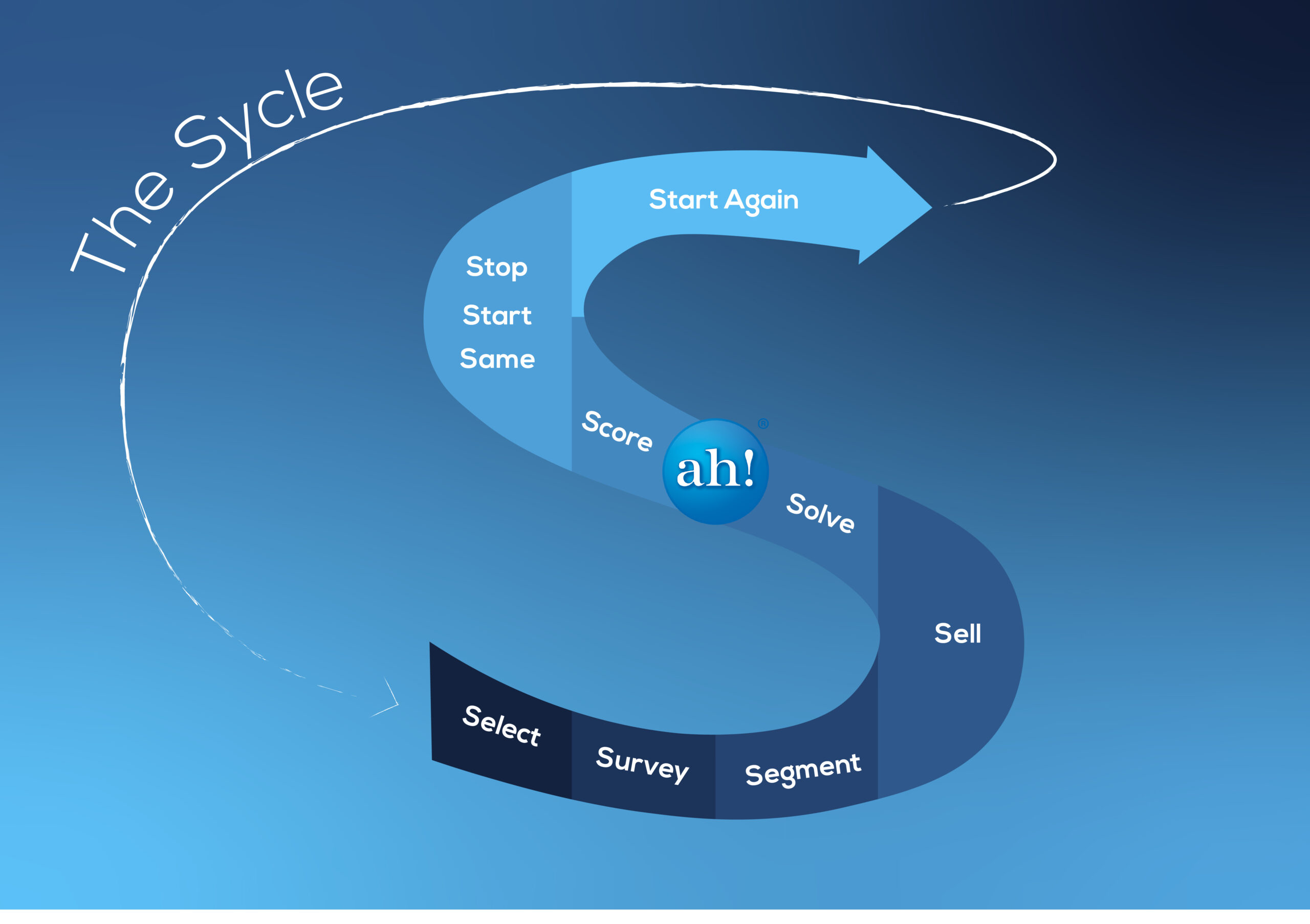
The third step in the Population Health Sycle (TM) (PHS) framework is Segment. This step involves dividing the population into subgroups based on shared characteristics. By segmenting the population, the group doing the population health program can develop targeted interventions tailored to each subgroup’s specific needs.
Segmenting the population can be based on various factors, including age, gender, ethnicity, socioeconomic status, geographic location, cost, clinical measures, genetics, readiness to change, and risk factors. For example, healthcare providers may segment a population based on age to develop interventions that address the specific health needs of children, adults, and seniors. Similarly, segmenting the population based on risk factors such as smoking, obesity, or chronic conditions can help identify subgroups that require targeted interventions.
Segmentation can also be based on social determinants of health, such as income and education level, access to healthcare, and housing  conditions. Understanding these factors can help identify populations at higher risk of poor outcomes, higher costs, or developing certain health conditions.
conditions. Understanding these factors can help identify populations at higher risk of poor outcomes, higher costs, or developing certain health conditions.
Segmentation can be done using a variety of methods, in the early days, typical programs segmented patients into low, moderate, or high-risk categories. The systems were very simple, for example, one hospitalization or 2 or more ER visits placed that individual in the high-risk category. Today, we can use a multitude of measures from the Survey Step and stronger analytic tools such as machine learning algorithms to better Segment the population. The ultimate goal of this process is to get to an N of 1, segmenting the individual into the right bucket so that the services provided in the later step, Solve, achieve the outcome desired. Segmenting is moving towards precision medicine.
Once the population has been segmented, healthcare providers and the broader team can develop targeted interventions that address the specific needs of each subgroup.
Segmentation can also help identify gaps in healthcare and other services and access. For example, if a subgroup has limited access to healthcare services, healthcare providers may develop interventions that focus on improving access to healthcare services, such as mobile clinics, telemedicine or transportation.
Segmentation and the initial information from the Survey Step can be used to evaluate the effectiveness of interventions. By tracking health outcomes for each subgroup, healthcare providers can determine which interventions are most effective and adjust interventions as needed.
In conclusion, segmentation is a critical step in the PHS framework for population health management. By segmenting the population, healthcare providers can develop targeted interventions tailored to each subgroup’s specific needs. Segmentation can be based on various factors, including age, gender, ethnicity, socioeconomic status, geographic location, cost, clinical measures, genetics, readiness to change, and risk factors. Segmenting the population is done using data analytics and in some cases machine learning algorithms, which can help identify patterns and relationships between different factors. By developing targeted interventions, healthcare providers can improve health outcomes for the population and reduce healthcare costs. The next step in the PHS framework is Sell, which involves engaging the population and promoting behavior change.
So whether you’re looking for assistance developing population health management programs, or improving one you already have contact us or call us at 904*613*1224.